Curricular Reform in Serious Illness Communication and Palliative Care: Using Medical Students’ Voices to Guide Change
Publication date: April 29, 2024
Purpose: To gather and leverage the voices of students to drive creation of required, integrated palliative care curricula within undergraduate medical education in Massachusetts, which is lacking in a majority of U.S medical schools.
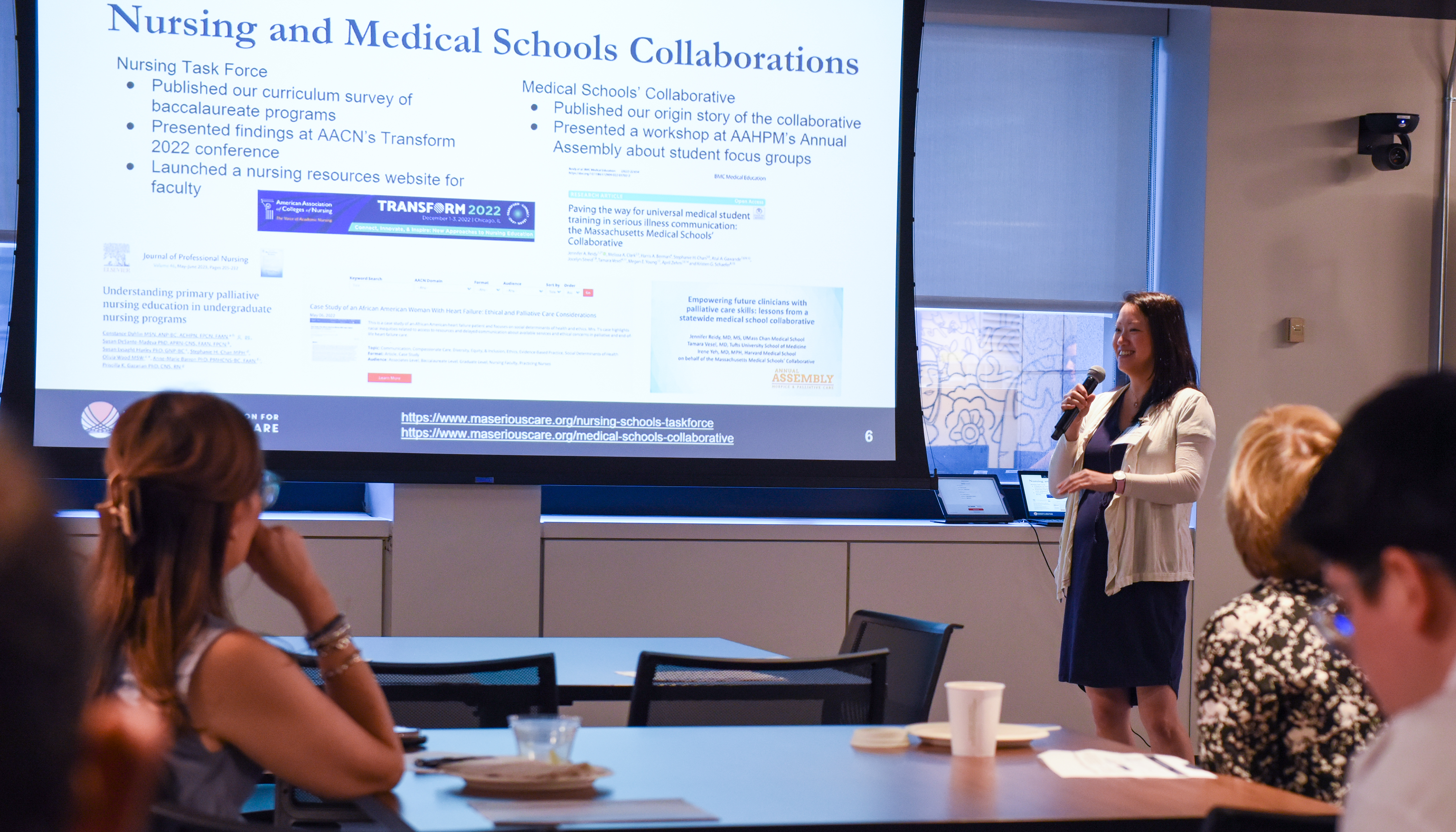
Method: The study was conducted by the Massachusetts Medical Schools’ Collaborative, a working group committed to ensuring all medical students in Massachusetts receive foundational training in serious illness communication (SIC) and palliative care. Eight focus groups groups (2 per participating medical school) were conducted during January–May 2021 and included a total of 50 students from Boston University Chobanian & Avedisian School of Medicine, Harvard Medical School, Tufts University School of Medicine, and the UMass Chan Medical School. Data collected from focus groups were discussed and coded. Themes were identified using the immersion/crystallization qualitative data analysis approach.
Results: Six key themes emerged. Students viewed SIC as essential to high-quality medical
practice regardless of specialty, and believed training in SIC skills and palliative care should be required in medical school curricula. Students preferred to learn and practice these skills using frameworks, particularly in real-world situations. Students recognized the expertise of palliative care specialists and described them as a scarce, often misunderstood resource in health care. Students reported iit was mostly “luck” if they were included in family meetings and observed good role models. Finally, students desired practice in debriefing after difficult and emotional situations.
Conclusions: This study confirms long-standing themes on students’ experiences with SIC and palliative care topics, including feeling inadequately prepared to care for seriously ill patients as future physicians. Our study collected students’ perspectives as actionable data to develop recommendations for curricular change. Collaborative faculty also created recommendations based on the focus group data for immediate and ongoing SIC and palliative care curricular change in Massachusetts, which can apply to medical schools nationwide.
