Leveling Up Communication with Irene Yeh

Publication Date: September 14, 2022
Meet Coalition working group member Irene Yeh, MD MPH, a palliative care physician at Dana-Farber Cancer Institute (DFCI) and Brigham and Women’s Hospital (BWH). Irene also serves as the Director of Medical Student Education for Palliative Care at DFCI/BWH and is a key faculty member of the Coalition’s Massachusetts Medical Schools' Collaborative. “My clinical work drives my interest in how we can improve communication with patients and family members. Sometimes the greatest challenges we face in the clinical setting stem from misunderstandings and miscommunications, especially with patients and families from different backgrounds,” said Irene. She is passionate about incorporating cross-cultural communication into medical education and across hospital departments.
Improving Cross-Cultural Communication
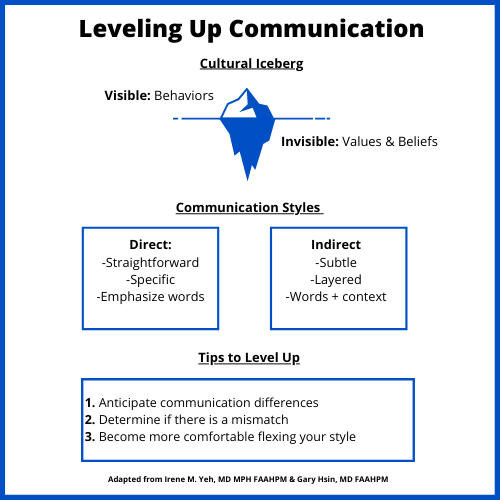
Irene’s work explores the role of cross-cultural communication and emphasizes its importance for building trust with patients. Effective communication can sometimes be challenging because people have different styles. Direct (low-context) communicators tend to be specific and detailed, with an emphasis on words to convey meaning. On the other hand, an indirect (high-context) communicator may share stories and rely on context, not just words, to get a message across. Differences in communication styles can lead to misinterpretation, assumptions, and judgment. For example, direct communicators might be seen as rude or abrupt whereas an indirect communicator may be interpreted as secretive or unknowledgeable. Furthermore, cultural backgrounds tend to influence communication styles. Irene shares the concept of a cultural iceberg where people’s behaviors are visible, but beliefs and values that drive behavior are often below the surface and invisible to others. Given that communication is a crucial component of patient care, Irene recommends thinking about communication mismatches and practicing different styles when facing a communication impasse.
New Palliative Care Clinical Immersion Experience for Medical Students
Irene is working to introduce palliative care to medical students earlier in their training. Harvard Medical School has a new, student-driven initiative where first-year medical students are now required to have a clinical immersion experience in hospice and palliative care. With support from other Coalition working group members Drs. Andrea Schwartz and Kristen Schaefer, in addition to Drs. Dorothy Tolchin and Kirsten Engel, Irene is leading the charge at DFCI/BWH, one of 8 sites for this educational program.
The clinical immersion experience starts with a 30-minute introduction to palliative care to describe different illness trajectories and models of palliative care and hospice. Then, the cohort of five students spends two hours shadowing palliative care clinicians in a way that doesn’t interrupt patient flow to see everything from talking to nurses, leading family meetings, formulating recommendations, and consulting with other clinicians. After the shadowing experience, the five students debrief with one of the attendings about their experience with special attention to the emotions they’re feeling and the emotions they witnessed from patients, family members, and the clinical teams. Opportunities to debrief were important findings of the focus group's research.
By the end of July 2022, 50 students will have completed the inaugural clinical immersion experience at DFCI/BWH. Faculty are collecting feedback from students and attendings on how it’s working. “The comments alone from the debriefing session after their shadowing experience confirmed why it was so needed. The students remarked how their concept of palliative care was different than what they saw in real-time and marveled about how palliative care fits into the context of standard care,” shared Irene.
Students at Harvard Medical School have other required clinical immersion experiences so the infrastructure was already in place to add this new one for palliative care and hospice. It’s exciting that this clinical immersion experience incorporates several key recommendations coming out of the Coalition's report from listening to medical students: incorporating serious illness communication earlier in training, making the activity required to take luck out of the equation, and regularly debriefing emotional clinical situations.
When asked why medical students aren’t usually taught about palliative care early in their training, Irene explains that medical students have so much to learn. It can be hard to consider the tradeoffs in medical education and how to pivot. Irene also shares that it took a long time for people to discuss the concept of palliative care. “There is a common fear that conversations about palliative care hasten death. However, healing is not just curing.”
